Anesthesia complications can sometimes lead to a cat’s heart stopping, a critical condition known as cardiac arrest. It is essential to understand the causes of these complications to prevent such life-threatening situations and ensure the safety of our feline companions.
During anesthesia, if a cat’s heart stops, immediate veterinary care is crucial. Bringing the cat to the nearest emergency clinic or veterinary hospital is necessary for specialized treatment, including cardiopulmonary resuscitation (CPR) and oxygen administration to restore normal heart rhythm and respiration.
There are various methods that veterinarians may employ to restart the cat’s heart during cardiac arrest. These include cardiac massage, chest compressions, and, in severe cases, open chest resuscitation with the administration of medications directly to the heart.
To minimize the risks associated with anesthesia, thorough pre-anesthetic evaluations should be conducted. This includes physical examinations, blood tests, and patient history reviews. Intraoperative monitoring of vital signs is crucial to detect any complications and ensure the cat’s hemodynamic stability.
In conclusion, understanding the causes of a cat’s heart stopping during anesthesia is essential for preventing cardiac arrest and ensuring the safety of our feline friends. By following established anesthesia safety guidelines and protocols, conducting pre-anesthetic evaluations, and providing vigilant monitoring, we can minimize risks and prioritize patient safety.
Key Takeaways:
- Cardiac arrest during anesthesia can be a life-threatening situation for cats.
- Immediate veterinary care, including CPR and oxygen administration, is crucial in cases of cardiac arrest.
- Veterinarians may employ methods such as cardiac massage, chest compressions, or open chest resuscitation to restart the cat’s heart.
- Thorough pre-anesthetic evaluations and intraoperative monitoring are necessary to minimize anesthesia risks.
- Prioritizing patient safety and following anesthesia protocols can help reduce complications and ensure optimal outcomes.
Immediate Veterinary Care for Cardiac Arrest in Cats
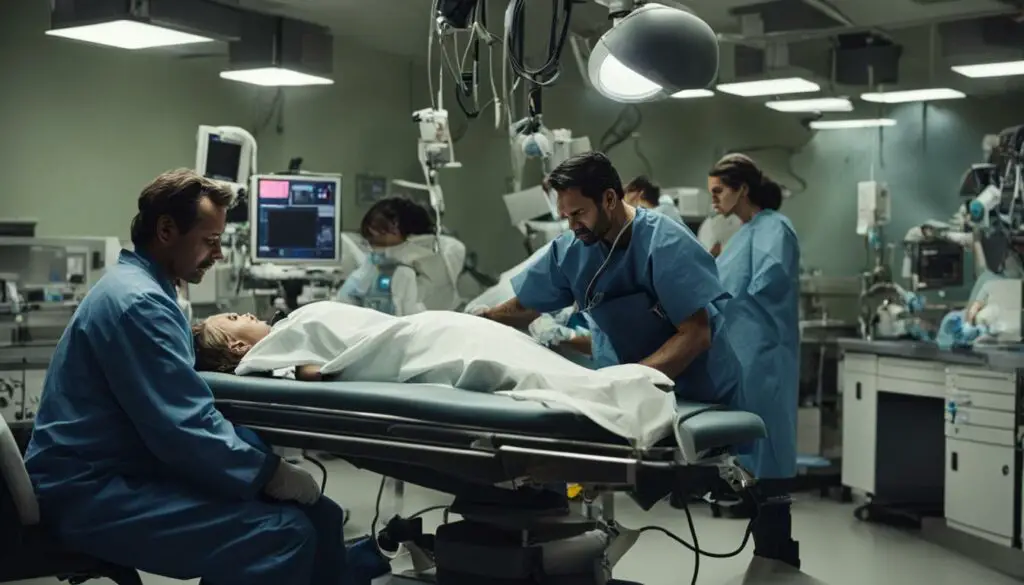
When a cat experiences cardiac arrest during anesthesia, immediate veterinary care is crucial. Owners should seek assistance from the nearest veterinary hospital or emergency clinic to ensure prompt treatment. In these specialized facilities, veterinary professionals have the expertise and resources necessary to address cardiac arrest effectively.
Upon arrival, the veterinary team will initiate cardiopulmonary resuscitation (CPR) to restore the cat’s heart rhythm and respiration. CPR involves a combination of chest compressions and artificial respiration, which can be lifesaving in this critical situation. Additionally, the team will focus on clearing the cat’s airways, ensuring adequate oxygen supply, and providing any necessary medication.
The objective of immediate veterinary care is to optimize the chances of a successful resuscitation and stabilize the cat’s condition. It is important to note that time is of the essence in these situations, and seeking professional help promptly can significantly improve the cat’s prognosis.
| Treatment Steps for Cardiac Arrest in Cats: |
|---|
| 1. Seek immediate veterinary care at a hospital or emergency clinic. |
| 2. Veterinary professionals will perform cardiopulmonary resuscitation (CPR) to restore heart rhythm and respiration. |
| 3. Airway clearance and oxygen administration are essential for optimal resuscitation. |
| 4. Medication may be administered to support cardiac function. |

I can’t emphasize enough the importance of immediate veterinary care when a cat experiences cardiac arrest during anesthesia. Time is crucial, and seeking professional help promptly can be lifesaving. Remember, veterinary professionals have the expertise and resources to perform life-saving interventions and restore your cat’s well-being.
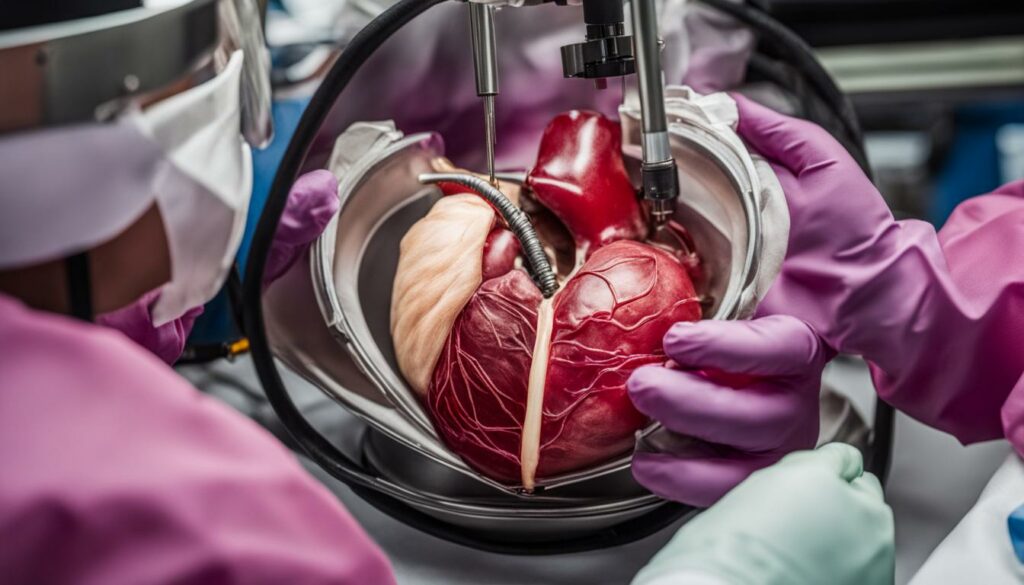
Methods to Restart the Heart During Cardiac Arrest
During a cardiac arrest in cats, when cardiopulmonary resuscitation (CPR) alone is unsuccessful in restarting the heart, veterinarians may employ additional methods to restore the heart’s function. These methods include cardiac massage, chest compressions, and open chest resuscitation.
Cardiac Massage
Cardiac massage involves applying pressure to the chest to stimulate the heart. By manually compressing the heart, veterinary professionals aim to restore its normal rhythm and circulation. This technique can be particularly useful in cases where the heart is unresponsive to CPR alone.
Chest Compressions
In some situations, chest compressions may be necessary to forcefully push the chest and restore heart rhythm. This technique involves applying pressure to the chest wall at a specific rate and depth, mimicking the natural squeezing action of the heart. Chest compressions can provide a vital lifeline in cases of cardiac arrest.
Open Chest Resuscitation
If cardiac massage and chest compressions are ineffective, veterinarians may need to perform open chest resuscitation. This involves making incisions in the chest and administering medications directly to the heart to restore its function. While more invasive, this technique can be a last resort to revive the heart and save the cat’s life.
It’s important to note that these methods should only be performed by trained veterinary professionals in a clinical setting. The success of restarting the heart depends on various factors such as the cat’s overall health, duration of cardiac arrest, and underlying conditions. Immediate veterinary care and prompt interventions are crucial in increasing the chances of a successful resuscitation.
| Method | Description |
|---|---|
| Cardiac Massage | Apply pressure to the chest to stimulate the heart and restore its rhythm. |
| Chest Compressions | Forcefully push the chest to restore heart rhythm. |
| Open Chest Resuscitation | Make incisions in the chest and administer medications directly to the heart to restore its function. |
Understanding Anesthesia and its Risks
Anesthesia is a vital component of many veterinary procedures, allowing for pain-free medical interventions. However, it is important to understand that anesthesia carries inherent risks for our feline companions. Adverse reactions can occur, ranging from mild effects such as swelling at the injection site to more severe complications like anaphylactic shock or even death.
One specific risk associated with anesthesia in cats is the potential for aspiration pneumonia. If a cat is not properly fasted before anesthesia, there is a risk of vomited material entering the lungs, leading to this life-threatening condition. It is crucial for veterinary professionals to ensure that all necessary precautions are taken to minimize the risk of aspiration pneumonia.
It is important for cat owners to have a thorough discussion with their veterinarian about the risks and benefits of anesthesia for their particular feline. By understanding the potential risks and taking appropriate measures to minimize them, we can ensure the safety of our beloved pets during anesthesia.
Factors to Minimize Anesthesia Risks
Ensuring the safety of our feline companions during anesthesia is of utmost importance. To minimize the risks associated with anesthesia, thorough pre-anesthetic evaluations are essential. This involves a comprehensive assessment that includes a review of the cat’s medical history, a physical examination, and blood tests to evaluate their overall health status.
Pre-Anesthetic Evaluation
Prior to administering anesthesia, it is crucial to gather detailed information about the cat’s health and any pre-existing conditions they may have. This includes conducting a thorough patient history to identify any underlying concerns that could impact the anesthesia process. By understanding the cat’s medical background, veterinarians can tailor the anesthesia protocol to minimize risks and provide individualized care.
Blood Tests
Blood tests play a vital role in pre-anesthetic evaluations. These tests help identify any abnormalities or underlying health issues that may not be apparent during the physical examination. By analyzing blood chemistry, liver and kidney function, and performing a complete blood count, veterinarians can assess the cat’s overall health and make informed decisions regarding the anesthesia plan.
Additionally, blood tests can detect other conditions that may increase the risk of complications during anesthesia, such as anemia or clotting disorders. Identifying these issues allows veterinary professionals to take necessary precautions and make adjustments to the anesthesia protocol to ensure the safety of the cat throughout the procedure.
Intravenous Access
Establishing adequate intravenous access is crucial during anesthesia to ensure prompt administration of medications and fluid therapy if needed. Intravenous catheters provide a direct route for delivering drugs and maintaining fluid balance, allowing veterinarians to respond quickly to any potential emergencies during the procedure. This access also facilitates the administration of medications that may be required to manage changes in blood pressure, heart rate, or other vital signs that may occur during anesthesia.
By prioritizing pre-anesthetic evaluations, performing necessary blood tests, and establishing intravenous access, veterinary professionals can minimize anesthesia risks and ensure the well-being of our feline companions throughout the procedure.
Table: Pre-Anesthetic Evaluation Checklist
| Pre-Anesthetic Evaluation Checklist |
|---|
| Gather detailed medical history |
| Perform a comprehensive physical examination |
| Conduct blood tests: |
| – Complete blood count (CBC) |
| – Blood chemistry panel |
| – Liver and kidney function tests |
| – Coagulation profile |
| Establish intravenous access |

Importance of Intraoperative Monitoring
During anesthesia, the continuous monitoring of vital signs is crucial for ensuring the safety and well-being of a cat. Intraoperative monitoring allows veterinary professionals to promptly detect any complications or deviations from normalcy, providing the opportunity for early intervention and adjustment of anesthesia protocols if needed. By maintaining hemodynamic stability throughout the procedure, the risk of anesthesia-related complications can be minimized.
Anesthetic monitoring involves the measurement and assessment of vital signs such as heart rate, blood pressure, oxygen saturation, and carbon dioxide levels. These parameters provide valuable information about the cat’s cardiovascular and respiratory status, ensuring that anesthesia is proceeding smoothly. Any significant changes in these vital signs can indicate potential complications, such as cardiac depression or inadequate oxygenation, allowing for immediate action to be taken.
Anesthesia complications can arise due to various factors, including drug reactions, inadequate ventilation, or inadequate perfusion. Intraoperative monitoring helps identify these complications early on, enabling veterinary professionals to address them promptly. By closely monitoring the cat’s vital signs throughout the procedure, any abnormal readings can be quickly recognized and appropriate interventions can be implemented to maintain the cat’s safety and optimize anesthesia outcomes.
| Vital Signs Monitored | Definition | Significance |
|---|---|---|
| Heart Rate | Number of heart contractions per minute | Indicates cardiac function and depth of anesthesia |
| Blood Pressure | Force exerted by blood against arterial walls | Assesses perfusion to vital organs |
| Oxygen Saturation | Percentage of hemoglobin saturated with oxygen | Reflects oxygenation status and respiratory function |
| Carbon Dioxide Level | Concentration of carbon dioxide in the blood | Indicates adequacy of ventilation |
By acknowledging the importance of intraoperative monitoring and diligently assessing vital signs, veterinary professionals can ensure the safe administration of anesthesia and minimize the risks associated with this critical aspect of veterinary care.

Postoperative Care for Anesthetized Cats
After undergoing anesthesia, cats require diligent postoperative care to ensure a smooth recovery and minimize the risk of complications. Close monitoring of vital signs and body temperature is essential during this critical period. Hypothermia, a condition where body temperature drops below normal levels, and hyperthermia, an elevated body temperature, are common postoperative complications that need to be promptly addressed.
During postoperative recovery, vigilant patient monitoring is crucial. Regular assessment of heart rate, respiratory rate, blood pressure, and body temperature allows early detection of any abnormalities or signs of distress. This monitoring helps veterinary professionals identify and address issues promptly, ensuring the cat’s well-being and reducing the risk of post-anesthetic complications.
“Postoperative care is a crucial phase in an anesthetized cat’s journey towards a successful recovery. It involves close observation and proactive interventions to maintain the patient’s stability and comfort,” says Dr. Smith, a renowned veterinary anesthesiologist.
Additionally, managing body temperature is paramount during the postoperative period. Hypothermia, characterized by abnormally low body temperature, can lead to delayed recovery and other complications. Conversely, hyperthermia, marked by excessive body heat, can indicate underlying inflammation or infection. Active measures, such as providing appropriate bedding and using heat pads or cooling devices as needed, can help regulate body temperature and support the cat’s recovery.
| Common Postoperative Complications | Signs and Symptoms | Treatment |
|---|---|---|
| Hypothermia | Shivering, pale gums, lethargy | Warming with blankets or heat sources, adjusting environmental temperature |
| Hyperthermia | Panting, excessive drooling, red gums | Cooling with damp towels or fans, providing fresh water |
Ensuring a cat’s postoperative recovery is a collaborative effort between veterinary professionals and pet owners. Following the veterinary team’s instructions regarding medication administration, diet, and activity restrictions is crucial to optimize the chances of a successful recovery.
Disclaimer: This article is for informational purposes only and does not replace professional advice. If your cat has undergone anesthesia, consult with your veterinarian for specific postoperative care instructions tailored to your cat’s condition.

Feline Anesthesia Safety Guidelines
When it comes to feline anesthesia, following proper guidelines is crucial to ensure the safety and well-being of our feline companions. The American Association of Feline Practitioners (AAFP) has issued comprehensive guidelines that serve as a valuable resource for veterinary professionals. These guidelines emphasize the importance of conducting thorough pre-anesthetic evaluations, establishing appropriate anesthesia protocols, and implementing effective monitoring during the procedure.
The feline anesthesia guidelines provided by the AAFP focus on the significance of a detailed pre-anesthetic evaluation. This evaluation includes a comprehensive medical history review, a physical examination, and a stress assessment. By understanding the cat’s overall health status, veterinarians can identify any potential risks or complications that may arise during anesthesia. This allows for the development of tailored anesthesia plans that prioritize patient safety and minimize the occurrence of adverse events.
Furthermore, the AAFP guidelines provide recommendations for appropriate anesthesia protocols specific to feline patients. These protocols encompass premedication, induction techniques, and intraoperative monitoring. The guidelines stress the importance of using medications that are safe and effective in cats, while also highlighting the need for vigilant monitoring of vital signs throughout the anesthesia process. By adhering to these guidelines, veterinary professionals can enhance the overall safety of feline anesthesia procedures and optimize patient outcomes.
Key Points:
- Feline anesthesia guidelines issued by the AAFP ensure the safety and well-being of cats undergoing anesthesia.
- Thorough pre-anesthetic evaluations, including medical history review and physical examination, are essential to identify potential risks.
- Appropriate anesthesia protocols, including premedication, induction techniques, and monitoring, minimize the occurrence of adverse events.
By following the feline anesthesia safety guidelines established by the AAFP, veterinary professionals can provide optimal care for their feline patients, ensuring a safe and successful anesthesia experience.

Anesthesia Risks Based on ASA Physical Status Classification
When evaluating the anesthetic risk for cats, veterinarians often rely on the ASA physical status classification. This classification system categorizes patients into different classes based on their overall health status, allowing veterinary professionals to assess the likelihood of anesthetic complications. Understanding the ASA classification is crucial in tailoring anesthetic protocols and precautions to ensure the safety and well-being of the cat during anesthesia.
The ASA physical status classification ranges from ASA I to ASA V, with ASA I representing a healthy cat and ASA V indicating a cat with severe systemic disease or uncontrolled conditions. Cats with more severe health issues or advanced age are at higher risk for anesthetic complications. By categorizing cats into these classes, veterinarians can anticipate potential risks and make informed decisions about the anesthesia plan.
For example, a cat classified as ASA I with no underlying health conditions would be considered low risk for anesthesia. In contrast, a cat classified as ASA III with controlled systemic disease, such as diabetes, may require additional precautions and monitoring during anesthesia. By considering the ASA classification, veterinary professionals can tailor the anesthetic protocol to the individual cat’s needs, minimizing the risks associated with anesthesia.
Anesthetic Risk Based on ASA Classification:
| ASA Classification | Risk Level | Examples of Health Conditions |
|---|---|---|
| ASA I | Low Risk | Healthy cat with no underlying health conditions |
| ASA II | Mild Risk | Cat with mild systemic disease, such as well-controlled hyperthyroidism |
| ASA III | Moderate Risk | Cat with controlled systemic disease, such as controlled diabetes or mild heart disease |
| ASA IV | High Risk | Cat with severe systemic disease, such as uncontrolled diabetes or moderate to severe heart disease |
| ASA V | Extreme Risk | Cat with severe systemic disease or uncontrolled conditions |
By incorporating the ASA physical status classification into the evaluation of anesthetic risk, veterinarians can better assess the overall health status of a cat and implement appropriate precautions during anesthesia. This classification system helps ensure the safety and well-being of feline patients, allowing for a smoother anesthesia experience and improved outcomes.
Pre-anesthetic Testing and Bloodwork
Before undergoing anesthesia, cats should undergo pre-anesthetic testing and bloodwork to ensure their overall health and detect any underlying conditions that may affect the anesthesia process. This step is crucial in identifying potential abnormalities and allowing veterinarians to tailor the anesthetic plan accordingly.
The American Association of Feline Practitioners (AAFP) guidelines recommend different levels of testing based on the cat’s age. For younger cats, retroviral testing and basic bloodwork may be sufficient. However, for older cats, more extensive testing, including thyroid levels and radiographic imaging, may be necessary to obtain a comprehensive health assessment. These tests help detect hidden health conditions and abnormalities that could increase the risks associated with anesthesia.
By conducting pre-anesthetic bloodwork, veterinarians can gather important information such as complete blood counts, blood chemistry values, and clotting profiles. These results help identify any abnormalities in organ function, blood cell counts, or coagulation parameters. Detecting these issues early on allows for appropriate adjustments to the anesthesia plan and the implementation of measures to minimize potential complications during anesthesia.
Pre-anesthetic Sedation and Premedication
Pre-anesthetic sedation and premedication are essential steps in ensuring a smooth induction and minimizing stress for cats undergoing anesthesia. These medications help calm the cat, provide pain relief, and facilitate a smoother transition into anesthesia. When choosing the appropriate drugs, veterinarians consider factors such as the cat’s medical history, age, and overall health.
One commonly used class of drugs for pre-anesthetic sedation is opioids. Opioids like buprenorphine and morphine have sedative and analgesic properties, helping to reduce anxiety and provide pain relief. However, it’s important to carefully calculate the dosage to avoid excessive sedation or respiratory depression.
While benzodiazepines have sedative effects, they are generally avoided in cats due to their potential to cause agitation. Instead, alpha-2 agonists like dexmedetomidine are often used for pre-anesthetic sedation. These medications help calm the cat and provide analgesia, but they require careful monitoring due to their effects on blood pressure and heart rate.
Benefits of Pre-anesthetic Sedation:
- Reduces anxiety and stress
- Provides pain relief
- Smooth transition into anesthesia
- Facilitates ease of handling during the induction process
Proper pre-anesthetic sedation sets the foundation for a successful anesthesia procedure. By carefully selecting the appropriate sedative and analgesic drugs, veterinarians can help ensure the well-being and comfort of their feline patients.

| Sedation Medication | Type | Benefits |
|---|---|---|
| Opioids (e.g., buprenorphine, morphine) | Sedative and analgesic | Reduces anxiety and provides pain relief |
| Benzodiazepines (e.g., diazepam) | Avoided in cats | Potential to cause agitation |
| Alpha-2 agonists (e.g., dexmedetomidine) | Sedative and analgesic | Requires careful monitoring of blood pressure and heart rate |
Pre-anesthetic sedation plays a crucial role in ensuring the safety and comfort of cats undergoing anesthesia. By tailoring the sedation protocol to each individual cat’s needs and closely monitoring their response, veterinary professionals can optimize the anesthesia experience and promote positive outcomes.
Anesthesia Induction and Airway Management
When it comes to anesthesia, the process of induction and airway management plays a crucial role in ensuring the safety of cats during medical procedures. Anesthesia induction involves using specific drugs to achieve unconsciousness and facilitate a smooth transition into an anesthetized state. Proper airway management is equally important to secure the cat’s airway and deliver anesthetic gases and oxygen effectively.
During anesthesia induction, one commonly used technique is endotracheal intubation. This involves inserting a specially sized tube into the cat’s trachea to maintain a clear airway and facilitate the administration of anesthetic gases. Proper intubation is vital to ensure the flow of oxygen and anesthetic agents while preventing the risk of regurgitation and aspiration.
Proper airway management during anesthesia induction is essential to ensure the safety and well-being of cats. By performing endotracheal intubation and maintaining a secure airway, veterinary professionals can effectively deliver anesthetic gases and oxygen while minimizing the risk of complications.
However, it is crucial to proceed with caution during intubation to avoid potential airway complications. Laryngospasm, an involuntary constriction of the vocal cords, can occur if the cat’s airway is irritated or stimulated during the intubation process. This can lead to airway obstruction and compromise the delivery of oxygen and anesthetic gases. Additionally, care must be taken to prevent tracheal tears, which can result from excessive force or improper technique during intubation.
Overall, anesthesia induction and airway management require skill, precision, and attention to detail. By following established protocols and guidelines, veterinary professionals can ensure a smooth and safe anesthesia experience for cats, optimizing patient outcomes and minimizing the risk of airway complications.
Conclusion
Ensuring the safety of our feline companions during anesthesia is of utmost importance. By following proper anesthesia protocols and guidelines, we can minimize the associated risks and promote patient safety. Thorough pre-anesthetic evaluations, including medical history, physical examination, and stress assessment, help identify any underlying health issues that may impact anesthesia outcomes.
During the anesthesia procedure, continuous monitoring of vital signs and maintaining hemodynamic stability are critical. This allows veterinary professionals to detect any complications or deviations from normalcy early on and make necessary adjustments to the anesthesia protocol. Postoperative care is equally important, with close monitoring of vital signs and timely interventions to prevent complications like hypothermia or hyperthermia.
By incorporating the recommendations set forth by the American Association of Feline Practitioners (AAFP), we can enhance the safety of feline anesthesia. The AAFP guidelines emphasize the importance of pre-anesthetic testing and bloodwork, appropriate premedication and sedation, and careful induction and airway management techniques. These guidelines provide valuable insights and strategies to minimize the risks associated with anesthesia.
Ultimately, it is our responsibility as veterinary professionals to prioritize patient safety and well-being. By implementing comprehensive anesthesia protocols and ensuring vigilant care throughout the entire anesthesia process, we can provide a smooth and safe experience for our feline patients.
FAQ
What should I do if my cat’s heart stops during anesthesia?
Seek immediate veterinary care and bring your cat to the nearest veterinary hospital or emergency clinic.
How is cardiac arrest in cats treated during anesthesia?
Veterinarians may perform cardiopulmonary resuscitation (CPR) and administer medication to restore the cat’s heart rhythm. Oxygen administration and airway clearance are also essential.
What methods can be used to restart a cat’s heart during cardiac arrest?
Veterinarians may perform cardiac massage, chest compressions, or open chest resuscitation. Medications can be injected directly into the heart to restore its function.
What are the risks associated with anesthesia in cats?
Adverse reactions can occur, ranging from mild effects to severe complications like anaphylactic shock or death. There is also a risk of aspiration pneumonia if a cat is not properly fasted before anesthesia.
How can anesthesia risks be minimized for cats?
Thorough pre-anesthetic evaluations, including physical examination, blood tests, and imaging, can identify underlying health issues. Special attention should be given to cats with pre-existing conditions, and intravenous access should be established for emergency drug administration.
Why is intraoperative monitoring important during feline anesthesia?
Continuous monitoring of vital signs allows for early detection of complications. This helps maintain hemodynamic stability and enables prompt adjustments to anesthesia protocols if necessary.
What should I expect during the postoperative care of an anesthetized cat?
Close monitoring of vital signs, including heart rate, respiratory rate, blood pressure, and body temperature, is essential for early detection of complications. Hypothermia and hyperthermia are common postoperative complications that require appropriate interventions.
Are there guidelines to improve feline anesthesia safety?
The American Association of Feline Practitioners (AAFP) has issued comprehensive guidelines focusing on pre-anesthetic evaluation, medication protocols, and intraoperative monitoring specific to cats.
How can the anesthetic risk for cats be assessed with the ASA physical status classification?
The ASA classification system categorizes patients based on their overall health status, helping veterinarians predict the likelihood of anesthetic complications. Factors like severe systemic diseases or advancing age may increase the risk.
Why is pre-anesthetic testing and bloodwork important?
Pre-anesthetic bloodwork can detect hidden health conditions or abnormalities that may impact anesthesia. The extent of testing varies based on the cat’s age and health status.
What is the role of pre-anesthetic sedation and premedication?
These medications help ensure a smooth induction and minimize stress for the cat. Opioids are commonly used for sedation and pain relief, while benzodiazepines are generally avoided due to their potential to cause agitation. Alpha-2 agonists require careful monitoring due to their cardiovascular effects.
What is involved in anesthesia induction and airway management?
Anesthesia induction involves using drugs to achieve unconsciousness, and proper airway management is crucial. Endotracheal intubation is commonly performed to secure the airway and deliver anesthetic gases and oxygen, avoiding potential complications like laryngospasm or tracheal tears.
What is the importance of anesthetic monitoring in cats?
Anesthetic monitoring allows for real-time assessment of vital signs, such as heart rate, blood pressure, oxygen saturation, and carbon dioxide levels. It helps detect any complications or deviations from normalcy, allowing for prompt adjustments to anesthesia protocols if needed.
Source Links
- https://wagwalking.com/cat/condition/cardiac-arrest
- https://www.dispomed.com/feline-anesthesia-protocol-side-effects-and-complications/
- https://vcahospitals.com/know-your-pet/anesthesia-for-cats








